Sent to you by subbu via Google Reader:
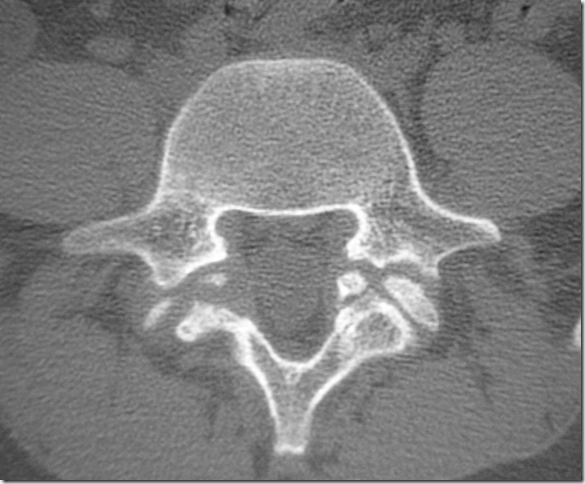
CT is currently the method of choice for guiding biopsy of lesions of the spine. However, in our hospital, fluoroscopy-guided percutaneous biopsy has been preferred for several years because of equipment availability and easy craniocaudal angulation. The aim of this study was to evaluate the efficacy of fluoroscopy-guided percutaneous biopsy in a clinical setting for diagnosing infectious spondylitis.
MATERIALS AND METHODS:A retrospective study was performed to evaluate 170 fluoroscopy-guided percutaneous biopsies in 140 patients (male/female = 70:70; mean age, 65.1 years; range, 16–89 years) in a clinical setting who were suspected of having infectious spondylitis between July 2003 and March 2010. Diagnosis was based on pathologic confirmation by tissue or culture from biopsy. The percentage of adequate specimens for diagnosis, histopathologic diagnosis for infectious spondylitis, and positive cultures for causative organisms were evaluated by retrospective review of medical records.
RESULTS:Adequate specimens for diagnosis were obtained in 165 of 170 cases (97.1%). The diagnosis of infectious spondylitis resulted in 134 of 170 cases confirmed through histopathology or clinical outcome (78.8%). In 51 of 134 cases (38.1%), the causative organism was confirmed by specimens from percutaneous bone biopsy. There were no biopsy-related major complications. The most common organism isolated was Mycobacterium tuberculosis (24 cases), followed by Staphylococcus aureus, Streptococcus agalactiae, and Streptococcus viridans.
CONCLUSIONS:Fluoroscopy-guided percutaneous biopsy is as accurate and effective as CT-guided biopsy for diagnosing infectious spondylitis.
Things you can do from here:
- Subscribe to Publication Preview using Google Reader
- Get started using Google Reader to easily keep up with all your favorite sites







 10:43:00 PM
10:43:00 PM
 Dr Subhash Kumar, MBBS, MD, DM
Dr Subhash Kumar, MBBS, MD, DM



















A.jpg)
A.jpg)
A.jpg)
A.jpg)

